
Xilma R Ortiz-González, MD, Ph.D.
Assistant Professor of Neurology and Pediatrics
University of Pennsylvania Perelman School of Medicine & Children's Hospital of Philadelphia
Ortiz-González Lab
Embracing the Journey
My journey began at the University of Puerto Rico in Cayey, where I majored in chemistry and minored in biology. Due to limited research opportunities available at the Cayey campus, I took the opportunity to participate in NIH-supported undergraduate summer research programs at R1 universities, such as the University of Wisconsin and University of Minnesota. These summer experiences were instrumental in exposing me to different career opportunities and sparked my interest in pursuing a research career. In particular, my time at the University of Minnesota was valuable because it introduced me to the physician-scientist career path. I was particularly captivated by the idea of researching mechanisms of disease while also interacting with patients, which led to my matriculation into their dual-degree MD and PhD graduate program.
For my PhD, I studied neural stem cell therapies by examining the neural differentiation potential of reprogrammed adult bone marrow cells in the mouse brain. This is something that is now well understood, but when I did my PhD, reprogramming somatic cells to a pluripotent state was a relatively new concept! During my graduate training, I was funded by both an NINDS F30 and a T32 training grant. These awards taught me about the NIH grant process and provided training opportunities that helped me hone my grantsmanship and manuscript writing skills which I have realized are critical for success in research.
Throughout my graduate training, I continued to make it a priority to take advantage of every opportunity to improve my writing. This skill development continued throughout my postdoc and fellowship. My mentoring team was key for me to develop this skill, as each member provided their unique perspective on writing. For example, you need someone who is a great writer, someone who can see the big picture, and someone who can review the science in detail. One person may not be good at everything, so it is important to assemble a diverse team of mentors to provide guidance. This mentorship team approach has not only helped improve my writing but has been crucial in learning to navigate the skillset needed to succeed in the physician scientist path.
After my MD/PhD training, I moved to Philadelphia where I did my residency at the Children’s Hospital of Philadelphia (CHOP). While here, I developed an interest in rare diseases and mitochondrial disorders in children, such as those that cause developmental regression (when skills such as speaking and walking are lost). I decided to stay at CHOP for my postdoc in mitochondrial genetics and trained through an NINDS K12 Academic Development Award in the lab of Dr. Doug Wallace. The K12 provided 75% protected time, which proved to be invaluable because it helped reduce my clinical load and gave me time to develop my own research program. Both the funding and Dr. Wallace’s mentorship was critical for my transition from a postdoc to a faculty position. This time allowed me to develop an independent research program and receive an NINDS K02 independent scientist award which ultimately allowed me to start my own lab.
The work in my lab is currently focused on understanding the mechanisms of ultra-rare neurodevelopmental disorders, including some linked to variants more prevalent in children of Puerto Rican ancestry. As a pediatric neurogeneticist, I see patients who have genetic differences that affect neurodevelopment. Most of these rare disorders don’t have therapies, and often little is known about the underlying mechanisms. As a physician-scientist, working with these patients may give us a window of opportunity to understand what these variants can teach us about the human brain and maintaining brain health. My research is driven by seeing first hand the devastating nature of these early-onset neurodegenerative diseases and the desire to find answers for them and their families.
While my academic and clinical journey may seem linear, there were certainly a few obstacles along the way. I remember one significant challenge was struggling with the uncertainty of succeeding at becoming an independent investigator as a physician-scientist. This struggle was exacerbated knowing the significant time commitment and training that is required to get to this point. The combined degrees take about 8 years, residency was an additional 5 years, with clinical fellowships and postdoctoral training piling on additional years. By the time you are competitive for a faculty position, it is close to a 20-year path. In addition to this, your income potential is limited during training, so it takes an extra toll for those who don’t have other means of financial support. Amidst this challenge, support from funding agencies like NINDS, particularly during the years of developing your research program and establishing your lab, were absolutely critical. You need to not only utilize the resources available to you, but it is also important to try to maintain a healthy work-life balance and continue to do things that bring you joy.
In addition to persistence and work-life balance, I would also say that success in research also requires maintaining your curiosity and resilience through all the challenges. Researchers are constantly dealing with failure and to get past this, they must be tolerant of frustration and embrace that this is part of the process. Having confidence is also extremely important, and understanding that the setbacks are all part of the process. I remind myself and my trainees that we need to separate our personal worth from the unfavorable academic outcomes, like not getting papers accepted or getting a bad score on a grant. It also helps when senior scientists with established labs talk about their own barriers and hurdles, so we all realize that setbacks or disappointments do happen to everyone.
I often advise trainees that throughout your training, you really to need make sure to enjoy your work and find projects that keep you engaged. Cherish the highlight (AHA!) moments, like knowing that you just may have discovered something that no one else knows. For me, it is also important to value your heritage and cherish who you are, particularly for those coming from backgrounds underrepresented in STEM. I often hear from Latinx PhD candidates and graduate school applicants that I am the first Latina faculty/PI that they have met. Being a visible role model is an immense privilege and I hope it helps trainees who come from underrepresented backgrounds to know that they can succeed in science too. This is an amazing career path; it is a long journey but there is something to be learned and enjoyed every step of the way!
Current Research
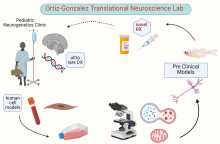
Dr. Xilma Ortiz-Gonzalez is physician-neuroscientist specializing in pediatric neurogenetics. She has contributed to establishing, functionally validating, and/or expanding the phenotypic characterization of over 20 monogenic rare neurodevelopmental disorders. Her research laboratory tackles the molecular mechanisms of pediatric ultra-rare disorders, particularly those in which mitochondrial dysfunction may contribute to neurodegeneration. She contributed to the discovery of TBCK as a novel disease human gene (PMID: 27040692) and to characterize the specific neurodegenerative course that includes progressive motor neuron disease in children with the Boricua variant (PMID: 29283439). Her lab first identified autophagic dysfunction as well as mitochondrial defects in patient-derived fibroblasts. Her team later showed that the mitochondrial respiratory defects in TBCK-deficient cells are likely secondary to lysosomal dysfunction (PMID: 34816123), since lysosomal acidification can rescue the mitochondrial phenotype. Currently, her laboratory continues to work on these questions: (1) What is the physiologic function of TBCK? (2) Why are neurons particularly susceptible to loss-of-function variants? (3) What is causing the lysosomal dysfunction that is presumably driving impaired mitochondrial quality control? Her lab also works in other pediatric neurodegenerative disorders that share secondary mitochondrial dysfunction as a common potential disease mechanism to understand how to better develop targeted therapeutics in the future.
