In last month’s NINDS Director’s message I introduced the planning stages of the NIH HEAL Initiative, Helping to End Addiction Long-term. After months of planning, the HEAL Initiative is being rolled out today in a Viewpoint published in the Journal of the American Medical Association. HEAL is a coordinated effort to support research in academia, industry, and healthcare that will help our nation respond to the opioid crisis we are facing.
HEAL will advance research to reduce the risks of opioid use and misuse, and will also reduce reliance on opioids by improving pain care. NINDS leads the NIH Pain Consortium’s 23 NIH Institutes and Centers whose mission includes improving the treatment of a variety pain conditions. Our focus in the HEAL Initiative will be in developing non-addictive pain treatments that may displace the need for opioids, and importantly, serve as effective treatments for acute and chronic pain conditions for which opioids are not effective. This work will be informed by partners from industry, academia, the Food and Drug Administration (FDA), and patients suffering from chronic pain.
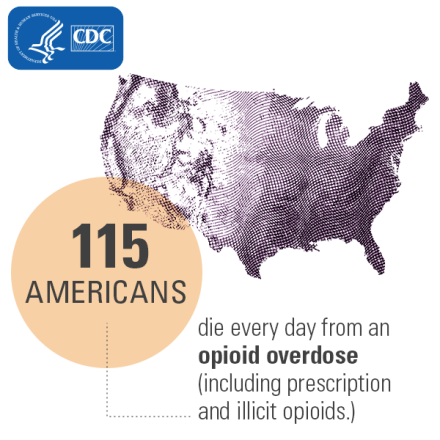
The dramatic increase in prescription opioids, which started in the 1990s, along with easier access to heroin and other illicit opioids such as fentanyl, has spiraled into the epidemic of addiction we face today. With 25 million people experiencing daily chronic pain in the U.S., it is imperative that we support research to advance both our understanding of the underlying condition and development of better treatments for those suffering. Here we list and briefly describe the pain research programs into which we hope to engage the research community. Please see the HEAL Initiative website for a complete description of the program, including funding opportunity announcements, as well as efforts by the National Institute of Drug Abuse to develop more effective treatments for addiction and prevention of overdose.
Understanding how to prevent chronic pain: The Acute to Chronic Pain Signatures Program
Chronic pain may develop over time from disease processes that damage nerves or other tissues, such as diabetic nerve pain or sickle cell disease pain. In some people chronic pain also can develop and persist after an acute injury or event. In most people pain resolves with treatment or after the injury heals, but in some it persists. We do not understand the biological factors that cause acute pain to lead to chronic pain. With support from the Common Fund, NIH will launch an intensive study of persons with an acute pain event such as surgery or trauma with the goal of identifying predisposing risk factors that lead to chronic pain, as well as targets for the development of therapies that can prevent chronic pain.
Discover and Validate Novel Targets for Safe and Effective Pain Treatment
HEAL will fund research to discover new therapeutic targets in the nervous system’s pain-related circuits. While the NIH will build on its core strengths in innovative basic science, HEAL also will enlist expertise from industry partners and the FDA to support the research required to determine the robustness of potential targets. For example, we will support studies on how the new targets’ effects on pain vary in different experimental animal models, or with age, sex, or in different pain conditions. As neural signaling pathways in the pain system are often employed in other brain circuits, it is important to identify ways to manipulate signaling precisely to reduce pain without causing adverse effects on other brain pathways. As one potential strategy to overcome this challenge, we will support investigation of devices that directly modulate circuit activity or that deliver medicines or other molecular interventions to specific pain system targets.
Engineering a Preclinical Testing Platform to Identify and Profile Non-Addictive Therapeutics for Pain
Disappointingly, over the years many agents that worked in animal models failed to show pain-relieving effects in clinical trials. Innovative means of rapidly screening potential treatments for their biological effects on pain targets would bolster the development of new treatments for a variety of pain conditions. In the HEAL Initiative, the National Center for Advancing Translational Sciences will (1) design human cell-based screening platforms that more closely approximate the human physiology of pain, addiction and overdose than currently available cellular and animal-based platforms; (2) use these platforms to identify pharmacological agents to probe potential therapeutic targets; and (3) accelerate studies of novel small molecule and biologic drug candidates for testing in humans. NINDS will develop a platform of animal models that more closely mimic a variety of human pain conditions to test non-addictive treatments (small molecules, biologics, natural products, or devices) for acute and chronic pain. By reducing the upfront economic burden for such preclinical screening and generating rigorous, high quality data, the program will incentivize the discovery of novel non-opioid, non-addictive therapies.
Translational programs in therapy development
NINDS has developed a variety of programs that support the design, implementation, and management of research activities critical to translational challenges in the treatment of neurological disease. The goal is to provide funding all along the therapy development pathway through to FDA Investigational Device (IDE) or Investigational New Drug (IND) Application, and even to Phase 1 clinical trials. Within the HEAL Initiative, NINDS will customize aspects of these programs for the development of non-addictive pain treatments. A suite of programs called Innovation Grants to Nurture Initial Translational Efforts (IGNITE) support early-stage therapy development, and programs such as Cooperative Research to Enable and Advance Translational Enterprises for Biotechnology Products and Biologics (CREATE Bio) and the Blueprint Neurotherapeutics Network (BPN) support later-stage development.
Discovery and development of biomarkers for pain
A major barrier to advancing new pain treatments is the inability to objectively measure the biological effect of a treatment in patients. In HEAL, NIH will fund research to discover and validate “biomarkers” that can serve as such objective measures that will help define patient populations for clinical trials. Ideally, these biomarkers will reflect the same biological effect in both animal models and humans so that their use in animal studies can more directly inform decisions on dose, duration, and means of administration in human trials. Validation is a critical step in biomarker development to determine whether a biomarker is reproducible across multiple studies, study sites, and different pain conditions. In collaboration with industry experts and the FDA, NIH will support both biomarker discovery and rigorous validation to accelerate high-quality pain research toward Phase 2 trials and beyond.
To date, the NINDS biomarker program has published funding opportunity announcements that encourage the validation of biomarkers for neurological conditions, and we issued a notice of special interest in projects to develop and validate biomarkers for pain and pain therapies. To enhance this program further, we will hold a workshop in early 2019, focused on best practices for biomarker discovery.
Clinical Trials Network on Pain Research (CTNPR)
The cornerstone of the NIH HEAL Initiative’s efforts to develop effective, non-addictive pain treatments will be a clinical trials network to accelerate new drug and device testing in early clinical trials for safety and efficacy (Phase 2 trials). Running a clinical trial on pain is complex and fraught with confounders due to the many different pain conditions and their frequent co-occurrence with other health issues, such as depression, anxiety, and sleep disturbances. In response, NIH will work with the academic, industry, and patient community to develop and incorporate useful biomarkers to improve the ability to determine whether a treatment is working through its expected biological target. The CTNPR will conduct validation studies of biomarkers in well-characterized patients with specific pain conditions to ready these cohorts for biomarker-informed Phase 2 studies. Small molecules, biologics, or devices will be solicited for testing from a wide variety of sources including academia, small business, biotech, large pharmaceutical and device companies, with emphasis on treatments for pain conditions associated with a high degree of suffering and limited effective therapies. We anticipate the CTNPR will be a learning environment that helps make clinical trials to test pain treatments faster and more efficient. Input from industry and the FDA will be critical in building a powerful network that can collect the kinds of data required for successfully handing off the most promising treatments to industry partners to complete development and bring new therapies to patients.
On top of these new initiatives, we also will leverage the strides made in neural technology development through the NIH BRAIN Initiative and the Stimulating Peripheral Activity to Relieve Conditions (SPARC) program. We have issued a notice to researchers that we welcome BRAIN Initiative grant applications with a focus on nociceptive and pain circuitry. Our chances of success in this effort are enhanced through the collaborative efforts of pain research within all of NIH and the Department of Health and Human Services through the NIH Pain Consortium and the Interagency Pain Research Coordinating Committee. We greatly appreciate the help of the pain research community in getting the word out about these initiatives and helping us achieve our goals to treat pain effectively and prevent addiction. The challenge is formidable, and the crisis calls on all those with good ideas and dedication to make an impact.
